Publications
The Advance Care Planning International Conference: Day 1
5 November 2025
By C Moore, Health Literacy Officer
At the end of September, I was able to attend the Advance Care Planning international (ACP-i) conference on the Gold Coast. In an ideal world, I would have been able to bring a bunch of consumer representatives with me, but since I couldn’t, I’ll share what I learnt. It was absolutely jam-packed, so I will be skimming over a lot of detail – if you’d like to know more, corner me at the next Members Forum!
If you’d like to read the abstracts for these sessions, the program is on the conference website.
Community Perspectives Panel
The conference opened with a panel of consumers and carers reflecting on their experiences – Annaliese Holland, Chris Hofmeyer and Christina Matthews.
Annaliese is a 25-year-old from South Australia living with a rare terminal condition. She spoke about how advance care planning has helped her take back control of her health care choices . As a young person, she has found that doctors haven’t always included her in conversations about her care or respected her wishes because of the stigma around death. Her main message was that “the thing that makes death terrifying is that we don’t talk about it.” Read more about Annaliese’s experience in this ABC article.
Chris and Christina have both cared for family members who have died. They spoke about their different experiences of planning that was done well, allowing people to die peacefully surrounded by loved ones. They also shared their negative experiences when doctors did not take the time to listen and support communication needs or ignored stated wishes not to have certain treatments. It showed the importance of decision makers as advocates for the consumer.
Key takeaways from the panel:
- Learning what is important to your loved one through conversations is often more important than documentation. Knowing who they are helps you make the right choice.
- Planning needs to be realistic to what the system can provide – don’t promise what the system won’t deliver.
- Doctors need to listen and respect when younger or relatively ‘well’ people choose palliative care. They also need to take the time to allow people to properly process information, however long that may take.
- Advance Care Planning still has a long way to go for young people, particularly those who have terminal illnesses other than cancer.
- Conversations should be started early – we should talk about Advance Care Planning the way we do organ donation. Clinicians need to know that raising Advance Care Planning early won’t ‘jinx’ the outcome for their patient.
- Clinicians need to support decision makers and involve them in conversations so they have enough information to make the choices needed when the time comes.
Keynote: The Evolution of Advance Care Planning
Professor Rebecca Sudore from the University of California San Francisco spoke about the evolution of Advance Care Planning (ACP). She started off with a bit of the history of ACP, which has been controversial as evidence has suggested it is ineffective – but all the evidence is based on older ‘check-box’ models, rather than conversations and values.
Rebecca shared the Care Planning Umbrella, a newer framework for advance care planning that focuses on:
- preparing for communication and decision-making,
- considers quality of life and what makes planning meaningful,
- present and future decisions tailored to your life stage.
To work well, this framework needs to factor in things like cultural values, life stages, different legal frameworks and supported decision making. She shared how her team tailored ACP programs for different cultures and life stages with research done with the Chinese, Latinx and Black communities in San Francisco. Some of the ways they tailored activities were:
- Supporting family and intergenerational decision making
- Awareness activities around Day of the Dead for Latinx communities
- Using a train-the-trainer model in Latinx communities so information could be shared by trusted community leaders
- Adapting messages for the Chinese community using the traditional five blessings
- Kitchen table conversation kits for the Black community to support conversations in safe spaces outside the health system
From our own experiences here in the ACT, we know tailored community-led strategies work, and it was great to see more research validating community-led Advance Care Planning activities.
Rebecca’s group has also developed and evaluated the PREPARE website and resources for consumers and carers. The entire website is written in an easy-to-read way with images, videos and translations. You can make a log-in and answer questions as you read through the information, giving you a report and draft advance directive to help you participate in planning discussions. It’s a very impressive tool, and there are several studies [1][2][3] showing it works!
Short sessions: Community Engaged Practice
I joined the presentation stream on community engaged practice to hear about campaigns and research programs that are working with consumers and communities to raise the profile of Advance Care Planning. These were the highlights:
- Development of advance care planning educational material after a community needs assessment in India – Dr Smriti Khanna, Hinduja Hospital And Medical Research Centre, Mumbai
Health care for life-limiting illnesses leads to serious financial issues for many people in India, and ACP is a very new process that is not well known. This project found that once people knew about ACP and medical directives, there was serious demand for more information. Based on consumer needs, they developed multilingual, health literate resources for ACP India. - Dying to Know Campaign: How communities embrace ACP; Insights and tips from the field! – Jessie Wiiliams and Danni Petkovic, Proveda
Dying to Know has expanded from just one day a year to a year-round community led campaign challenging the stigma around death and dying. They showed off the many different kinds of community events that formed this year’s campaign.Grant applications are open now for 2026 to support community led events and projects! Volunteers and diverse community groups are strongly encouraged to apply (and if you do, tell us so we can spread the word!)
- A youthful approach to end-of-life care decision making and advance care planning – Danielle Clarke and Danielle Jacobs, Dying with Dignity Victoria
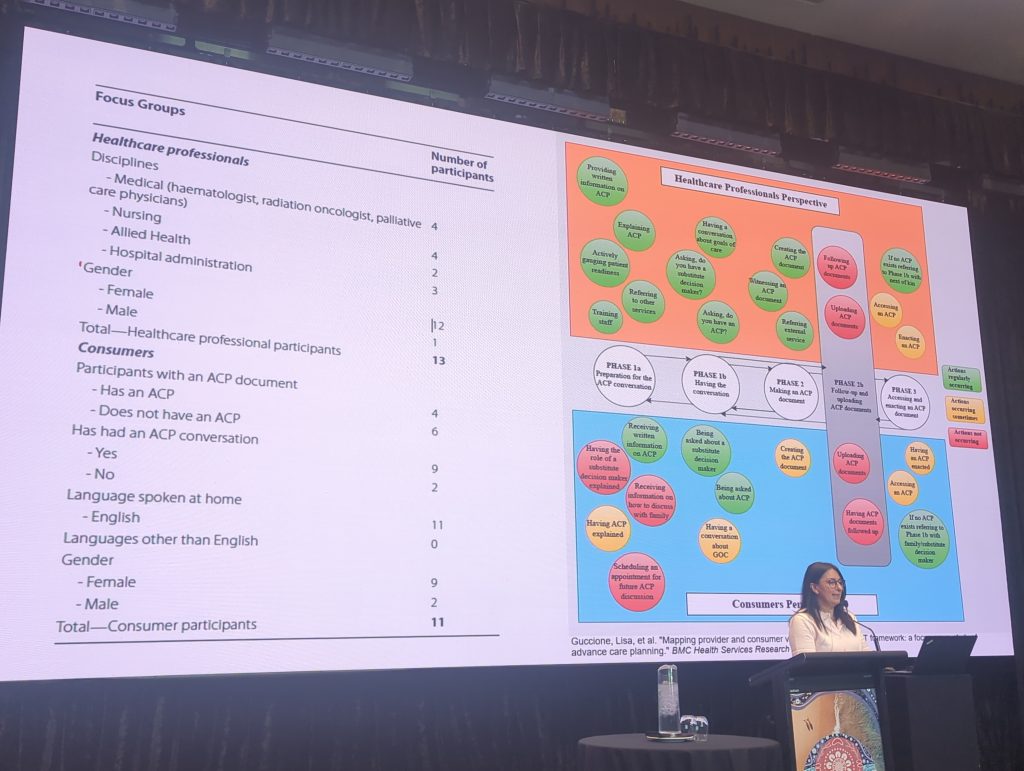
Dying with Dignity Victoria spoke about their Young Ambassadors program. They quickly found that young people weren’t just interested in Voluntary Assisted Dying (VAD), they also wanted better information and awareness about all end-of-life options. Because of how different young people’s end-of-life experiences are, they ended up totally reimagining their approach, making space for young people to design and lead the programs with their support. - Bridging gaps in advance care planning: implementing sustainable practice change through provider and consumer alignment – Dr Lisa Guccione, Peter Maccallum Cancer Centre
This study mapped out where the expectations of consumers and clinicians did not match up in the Advance Care Planning process. I found this chart (see photo) very interesting – it showed where consumers and clinicians had different expectations of who would be doing what and how that led to a breakdown in the process – check out the paper for more.
My key takeaway from these sessions was that many communities want more information about planning ahead and end-of-life care options, but stigma and confusion stop both consumers and professionals from starting and completing the process. This reinforced the importance of our work to raise awareness and demystify this process as much as possible!
Plenary: Future Care Yarning: A Culturally Grounded Approach
Cindy Paardekooper, National Aboriginal and Torres Strait Islander Palliative Care Association
Aboriginal and Torres Strait Islander people have worse health outcomes than non-Indigenous Australians. Communities are repeatedly traumatised by deaths that are not supported well.
Some of the barriers for Aboriginal and Torres Strait Islander people are:
- Processes relying on forms, where traditionally information is shared through yarning
- Different legal systems and forms across states
- Lack of trust in the system due to racism, trauma and unmet care needs
- Reluctance to talk about death and dying
- Split care between lots of different services that only address single issues
- Use of language like ‘Palliative Care’ and ‘Advance Care Directive’ that comes from unsafe health and legal systems
Cindy talked about how they are working to redefine palliative care as ‘Comfort Care’ and speak about care more holistically, so it includes cultural and spiritual needs. They use ‘normalised yarning’ to have conversations about end-of-life beyond just health care and completing documents. This approach means:
- Families making decisions together and at their own pace
- Having continuous dialogue, not just a single point in time
- Letting kinship systems guide care
- Including cultural knowledge holders
- Supporting the person, family and community all the way through death and after
This supports self-determination, affirms cultural identity and supports healing for the family and community.
Plenary: From Safari to Sanctuary: Reimagining Advance Care Planning Through an African Lens of Compassion
Dr Christian Ntizimira, African Centre for Research on End-of-Life Care
Christian spoke about his journey to become a surgeon and then a palliative care specialist in Rwanda after the genocide as a way to help his country to heal. He developed ‘the Safari concept’ as he found families were excluded from decision-making in existing models as they did not support the many varied family structures he saw. In Rwanda, decision making might not be done by a person we’d think of as ‘next of kin’ but is done collectively. It may be led by the eldest person, or a younger person with more influence, or the ‘lioness’ of the family as more women are taking on leadership.
Good communication with families relies on doctors to know how to meet the needs of families with:
- Multiple different religions and cultural backgrounds
- More traditional beliefs vs more progressive
- Impacts of intergenerational trauma
Christian’s concept uses animals to describe how different families behave or ‘suffer’ together and pairs that with practical ways that clinicians can change their communication approach to support them. This honours the different relationships, cultures and beliefs rather than expecting them to fit one particular model.
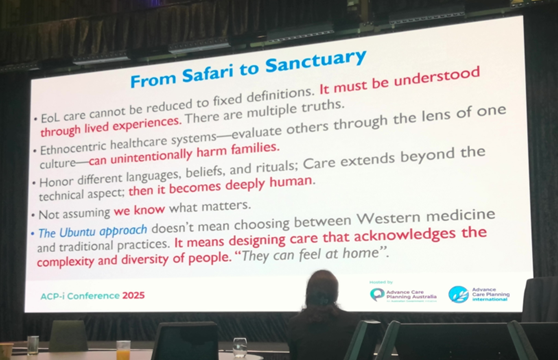
I found this approach so different to what I’ve seen before and can see some lessons to be learned here. I’ve grabbed a copy of Christian’s book for the office library.
Short sessions: Contemporary ACP, Ethics, Law and Human Rights
These sessions really underlined the ethical and legal need to fully inform people of their choices and what can be done to enact their right to equality in decision-making. Here are the key takeaways:
- Should Voluntary Assisted Dying (VAD) be raised in ACP – legal and ethical considerations – Professor Ben White, Queensland University of Technology
Ben outlined different regulations of VAD discussions – from banning clinicians from raising VAD at all, to mandating discussion when clinically appropriate. He argued that legal mandates may hinder informed decision-making. He suggested that a more ethical approach to ACP is one that supports consumers to have good conversations about all their end-of-life choices. - What’s supported decision making got to do with Advance Care Planning? – Dr John Chesterman, Queensland Public Advocate and Ms Theresa Flavin, consumer and human rights advisor
John highlighted that supported decision making is fundamental to realising the human rights of people with disability. Theresa shared her lived experience as a person with disability, highlighting barriers like assumed lack of capacity, inaccessible information, lack of time and rigid templates. She advocates for layered, fact-based conversations and the development of ‘Advance Social Directives’ covering identity, relationships, and values beyond just health. - Resolving post ACP disputes in South Australia: Elder inclusive mediation in shadow of the law – Mrs Shona Tostevin, Office of the Public Advocate, South Australia
Shona talked about how SA’s mediation model for ACP disputes has helped older people and their families. Since 2014, mediation has replaced tribunal hearings for guardianship cases, centring the person’s voice and values. This means fewer people are having their choices decided by tribunals and are able to retain their autonomy. The OPA also has an impressive toolkit for decision makers. - The Advance Care Planning conversation – where are we heading? Possible directions from ethical analysis – Prof. Dr. Georg Marckmann, LMU Munich
Georg explored how ethical analysis can help improve ACP processes. He stressed the importance of using specific scenarios in conversations to make sure stated values matched specific decisions.
Dinner: Is AI the future of Advance Care Planning?
At dinner we were shown an example of an Artificial Intelligence (AI) tool for Advanced Care Planning. This tool was called “Doctor Ellie”, and it was designed to have ongoing conversations with people about their wishes. After a day filled with speeches about the importance of conversations with decision makers and health care workers, it was quite jarring to hear about swapping them for an AI bot. Thankfully, I wasn’t the only one who thought so and this provoked lots of thoughtful conversation.
My main thought on this was that surely there are other ways we can use AI to improve planning other than removing the human element from these deeply personal conversations. Wouldn’t it be better to use AI to document conversations more accurately, or have an AI tool that doctors can ask about your plans to help them make decisions in line with your values?
And that was Day 1! Stay tuned for day 2 & 3 in a couple of weeks.

