Publications
The Advance Care Planning International Conference: Days 2 and 3
9 December 2025
By C Moore, Health Literacy Officer
This is part 2 of this blog post, recapping the many things I learned at the ACP-i conference. If you want to read more about the presentations, the Abstracts Book from the conference has now been published. It covers all the short sessions, including the ones I missed.
Day 2
Plenaries: The Art and Science of Communication
The science of the art: Conversation analysis and advance care planning – Associate Professor Stuart Ekberg, Flinders University
Many of the other sessions highlighted the importance of conversations in the Advanced Care Planning (ACP) process, so it was very helpful to see research into those conversations. Conversation analysis is an approach that looks at recordings of social interactions to analyse them in-depth on a case-by-case basis and look for common features.
Stuart’s team are applying this approach to ACP conversations between clinicians and consumers. Some of the features of the conversations they looked at were:
- Linking previous conversations with patients and their families, reflecting that ACP is an ongoing process.
- Using hypothetical scenarios to check that they understand how their stated wishes would apply in that situation.g. “would you still want this intervention in case of a heart attack?”
- Talking (in general terms) about other people’s choices to help individuals find what works for them.
Conversation analysis is a way to work out what good ACP conversations look like. It builds more meaningful evidence for improving health worker skills and measuring outcomes. It is also a way of understanding the complexity of ACP conversations, allowing for comparison across cultures, countries and professions.
Finding the Words: Supporting Communication and Decision-Making in Advance Care Planning – Dr Laura Chadha, Senior Speech-Language Pathologist & Research Fellow, Victoria University
Communication tools and techniques used in speech pathology can help people with communication difficulties to take part in shared decision making about their care. However, speech pathology has only recently been considered in palliative care, which has prevented people from sharing their choices.
Laura shared some practical ways to help make ACP conversations more accessible for people with communication challenges:
- Use strategies like chunk and check, checking for understanding (e.g. Teach Back) and visuals.
- Use multimodal tools like communication boards, symbol sets, gestures and devices – get help from a speech pathologist if needed.
- Allow extra time to process choices and share information in writing.
- Share decision aids like option grids and question lists – people could point to options to ask for more information.
She also spoke about how to support people with cognitive difficulties (like dementia) to take part in decision-making by using the SPIKES protocol and three-talk model of shared decision making considering the impacts of things like time of day and medications.
“The way other people treat me – they don’t understand ABI behaviour” Advance Care Planning in the context of acquired Brain Injury (ABI): Lessons learned from the experiences of the person and those who support them. – Professor Emeritus Jacinta Douglas, La Trobe University Melbourne
Jacinta’s research looks at the experience of people with acquired brain injuries and how to better support planning and decision making when people have cognitive changes that affect communication, memory and executive function.
Support for decision making enables people with cognitive disability to take part in their own decision making. It must be tailored to the individual and the situation and be flexible depending on the decision and support needed at that time. Decision making supporters need the right skills and knowledge to do this properly, so they have developed an evidence based practice framework to help develop effective support:
E-learning modules and resources for clinicians are available on the website Support for Decision Making. Another resource, Enabling risk – putting positives first, was developed for disability support workers, focusing on supporting people make choices that may involve risk.
These three sessions pulled together some great lessons on person-centred communication. We have been recommending some of these tools to health care workers for years and it is good to see them applied to ACP. I hope to see more work to translate the research into practical tools for consumers, families and decision supporters.
Short Sessions: Population Perspectives
These sessions focussed on uptake of ACP at a population level. You can have a look at each study for all the stats, but there were a few things that jumped out at me across each of them.
- A national prevalence study of advance care planning – Catherine Joyce, Advance Care Planning Australia
This is the first Australia-wide study of ACP uptake – you can see the full breakdown of their findings here. A few stats stood out to me: Of the people surveyed, only 13% had appointed a legal decision maker but a further 17% knew who they wanted to make decisions, but had not completed the legal forms. 27% of those that had not completed ACP said that they trusted their loved ones to know what they want. - Socio-demographic and clinical factors affecting advance care planning: large community longitudinal cohort in NSW, Australia
An interesting fact coming out of this talk – people with a current partner were more likely to have done some sort of ACP, but less likely to have completed an Advance Care Directive. Women, carers, people with chronic health conditions, and people needing support for daily activities were all more likely to have a directive in place. You can read the full results here. - Mirror of the mind: How personal preferences shape perceptions of partners end-of-life wishes – Dr Clement Meier – University of Lausanne
This study used data from a survey of older couples in Switzerland to look at how well people could predict their partner’s end-of-life wishes. They found that where people had different wishes from their partner, they were much less likely to correctly predict what their partner would choose. This was still the case even when they had completed Advance Directives! This reminds us how important it is to discuss your values as part of ACP, and not to assume your partner knows what you want.
Taken together, these sessions reminded me of this video – Love Is Not Enough – which I often show to groups to remind people that we can’t expect our loved ones to just know our wishes. We need to talk about our values directly and document them!
Short Sessions: Culturally Responsive Approaches
- Perspectives on advance care planning among family members of older Turkish and Moroccan adults – Prof Demirkapu Hakki
This study looked at low uptake of ACP in migrant communities in Belgium. Barriers to ACP included complex family relationships, emotional difficulties for family, and believing it was not urgent. Things that helped included information in native languages, GPs starting discussions and involving several family members to avoid conflict. I learned about the ‘foreign language effect’ where people may make more utilitarian decisions when speaking a foreign language – another reason why interpreting and translations are so important to shared care. - Cross-Cultural Acceptability Of The Serious Illness Conversation Guide Amongst Oncology Healthcare Professionals In South Africa – Dr Henriette Burger, Head of Division, Radiation Oncology, Stellenbosch University And Tygerberg Hospital
The Serious Illness Conversation Guide is commonly used in Western health care settings, but when tested in South Africa, they found that many of the prompts were not useful. One issue was the focus on individual autonomy rather than collective decision-making. Another was assuming choices are not restricted by cost or access. However, South Africa has high unmet needs for palliative care and this shows the importance of tailoring ACP tools for the cultural and system context. - Creating a CPR patient information leaflet without mentioning CPR, Dr Tammy Pegg – Cardiologist, NZ
Tammy spoke about some of the myths about CPR (covered in this podcast) and setting out to make resources about that. But when asked, consumers don’t actually want information about CPR, they want respect, support and empowerment. This led to a consumer empowerment resource and guide for clinicians on how to have better conversations. ACP NZ have many great resources, including co-designed resources for Maori and Samoan communities and Easy Read ACPs. - We need to know before you go – Planning Ahead for Sad News & Sorry Business – Miss Eliza Munro, Sorry Business Consultant, Ngiyani Wandabaa
Eliza spoke about this new resource kit developed to support culturally safe future care yarning. The kit includes teabag pouches, a set of 8 questions and a booklet to document choices. The resource can be used in community and by health workers to start early conversations, dispel myths and share knowledge with people and families. It can be ordered from Advance Care Planning Australia.
These sessions spoke to the importance of understanding how consumers from different communities view and speak about serious illness, life-prolonging treatments and death. It’s not just about translating information, but about finding out what is important in that culture and how it informs decisions.
Plenaries: Embracing the Journey
The most important part of the conversation…. Is the conversation – Dr Louis Peachey
Dr Peachey is a Girrimay and Djirribal man from the Djirribaligan people of North Queensland and a practicing GP. He spoke about how one of the issues with getting non-Indigenous doctors to deliver culturally safe end-of-life care is that they are so worried about breaching cultural protocols that they would rather not try. He encouraged simply starting the conversation and listening – “Listen to the words of the patient, listen to the silence between the words and remember that the beauty of a conversation is that no-one person has to have the answer.”
He spoke about how western culture’s aversion to death projects fears on Aboriginal people that they don’t necessarily feel. The expectation of fear around death makes it hard to start and continue the conversation but he also noted that doctors are always talking about death in some way – e.g. counselling someone about quitting smoking is ultimately linked to death – so maybe it is not as hard as it feels.
Are we where yet? – Cari Borenko, Fraser Health Authority, Canada
Cari’s response to the theme of “Are we there yet?” was “Are we where?”. She recounted a 30 year journey of “building the road as you go” as she built an ACP program from a single office to a system level ACP framework before there was anything like that in the literature. Some key takeaways for me:
- Training alone isn’t enough to embed ACP, it needs constant follow ups and buy-in from leadership. One way to get this is to co-facilitate a follow up session with leadership to talk about improving the system.
- Understanding where ACP is reported in the organisation can help you find the barriers and enablers – e.g. if ACP is sitting in a department focused on inpatient care, how do you prioritise community outreach?
- You have to listen to your community to understand the impact of ACP – it’s not reflected in the number of forms completed.
- How do we bring ACP into community? Find a table where you can connect to people and get invited into communities, don’t wait for them to come to you.
- Take the time to look back at the bumps, potholes and detours on the road you’ve been building and learn from them.
Even after three decades, there’s not a clear end in sight, but there’s definitely been progress. This made me reflect on the long-term experience of consumer advocacy and how often we don’t know what the end destination is as we push for incremental improvements. However, it is very important to stop and look back at the road we’ve built so we can learn and keep going.
Day 3
Plenaries: Systems Thinking
The Gift of Certainty: A Story About Love, Loss, and Advance Care Planning – Ms Courtney De Kever, Senior Director, First Nations Health Office, Australia
Courtney told us the story of her Nana, a proud advocate and activist for Aboriginal Justice, who had a well-planned, supported and culturally safe experience. The things that made the process safe for her Nana were:
- Giving space, respect and time for them to plan as a family
- Seeing her Nana as a whole person – an elder, a mother, a matriarch and a knowledge holder
- Recognising that dying is not just a medical process, but a spiritual event
- Supporting return to country
- Making space for stories, silence and questions
This meant that her Nana’s death was calm, well-planned and honoured her life. Courtney explained that dying on their own terms is an act of Sovereignty – an important reminder of why inclusive ACP is about more than just health care choices.
Her story really illustrated how systems that enable culturally safe planning and end-of-life care help people, families and communities find peace and healing. It also showed that good culturally safe end of life care is not a far-fetched idea – it is possible and can be spread further.
Establishing a digital advance care planning system from the clinical ground up – Prof Liz Reymond, Co-Director of Statewide Office of Advance Care Planning (OACP)
Queensland has a statewide Office of Advance Care Planning and with this, a statewide ACP tracker. The system was built with clinicians to make ACPs accessible across health services, and it means consumers can lodge their ACP once and expect it to be available. Clinician can even add comments about ACP conversations to the tracker and these are included in discharge summaries to support ongoing planning.
To evaluate the system, they ran an audit of 600 people to see if the care people received matched their Statement of Choices. They found that people who have completed a Statement of Choices are more likely to die out of hospital, with 80% dying in the place chosen on their plan. They also found that for this group, their stated choices for CPR were followed 100% of the time and 99% for life prolonging treatments. A larger study (~17000 people) showed that people completing ACP more than 6 months before they died were much less likely to present to emergency or be admitted to ICU.
This shows just how much a well-integrated system can enable consumers’ wishes to be followed. A comment from the audience pointed out how much culture has changed and that more health professionals recognise the importance of these documents, but the national systems need to catch up. This led neatly into the next speaker…
Digital Health in Advance Care Planning: Bridging Gaps, Building Trust – Mrs Karen Booth, Chief Clinical Adviser – Nursing, Australian Digital Health Agency
Karen took us through how the new Share by Default legislation was one of the biggest enablers of a nationally connected health care system, and 60-70% of pathology and diagnostic imaging results are now available on My Health Record and my health app.
However, for ACP there are major barriers due to the different laws between states and territories. But the consensus is that law reform is too slow and we have to find digital solutions to share ACPs across state borders. While you can currently have your ACP uploaded to your My Health Record and share it using the app, this does not mean a health service can access it on their own system. They are working toward integration with state and territory systems, but this is a few years away.
Short Sessions: Systems Challenges and Enablers
These sessions were all focused on the systemic approaches that can support ACP on-the-ground
- Empowering Communities: Local Government’s Role in Advance Care Planning Through Digital Resources – Ms Judith Lowe, Project Officer Independence And Wellbeing, City Of Onkaparinga (SA) & Ms Julie Wilhelm, Adelaide Hills Council
In South Australia, the My Future My Way program got Local Governments to train and support volunteers to improve ACP uptake. This included online resources and training to deliver peer-led workshops that could be adapted for diverse communities. Now, South Australia has the highest ACP engagement rate in the Country! Check out the project and resources here. - What’s the difference and the impact? Review of NFR policy and documentation across NSW health – Mr Douglas Billing, Clinical Nurse Consultant CPR Coordinator, Royal Prince Alfred Hospital
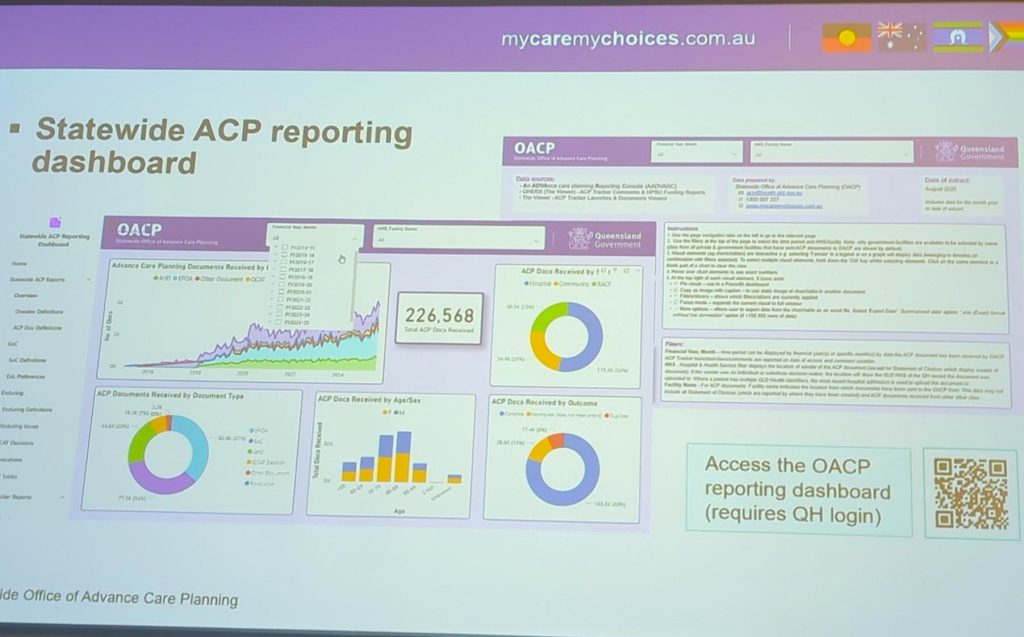
This session looked at all the different documents and policies across NSW Health that cover “Not-for-Resuscitation” orders. They found that most facilities do not have a dedicated policy, and there can be big differences between facilities. This, combined with staff rotations and patient transfers, means that ACPs and resuscitation orders are not consistently discussed and followed. This may lead to unwanted CPR and increased trauma for patients, families and staff. - How the Statewide Office of ACP, ACP Tracker and related systems support ACP in Queensland – Ms Leanne Clemesha, Nurse Unit Manager, Statewide Office Of Advance Care Planning (OACP)
This session dug in to how the OACP uses their tracker and reporting tools to ensure quality of ACPs. They have detailed reporting across the state (see photo below for a peek at their dashboard). They also review documents before uploading to make sure they are in the correct format and legally witnessed. Issues can then be followed up with individuals to fix any discrepancies and they can also provide education to health services and groups that help complete these documents, like Justices of the Peace.
- What impact do ACP legislative frameworks have on digital health system reforms in Australia? – Mrs Mila Obucina, Advance Care Planning Australia
This session took us through the differences in ACP law between states. These include whether a doctor must sign it, who can be an authorised witness, how health attorneys can be appointed and what decisions/values are recorded on the forms. This makes it very difficult to create one digital system for ACP that will be legally recognised (and practical for health services) nationwide.
Day 3’s sessions really drove home the system changes are needed to enable quality and actionable ACPs. That means greater flexibility in processes to allow culturally responsive planning, better systems to record values and choices along with changes to laws to make borders less of a barrier.
Closing
This was the first conference I’ve been to where the closing address was delivered by poem (and a tearjerker at that). Dr Craig Sinclair wrote it during the conference about the stories heard, lessons learned and the challenges still to come.
Personally, I learned lots about the history and impact of Advance Care Planning, ways to engage different communities and how to meaningfully measure outcomes. It highlighted how much more we could be doing in the ACT if we had a clear system-wide strategy with more resourcing to support community-led education and integrate ACP into systems across care settings.


